New study reveals that the malaria parasite can infect you as deep as your bone marrow
06/24/2018 / By RJ Jhonson

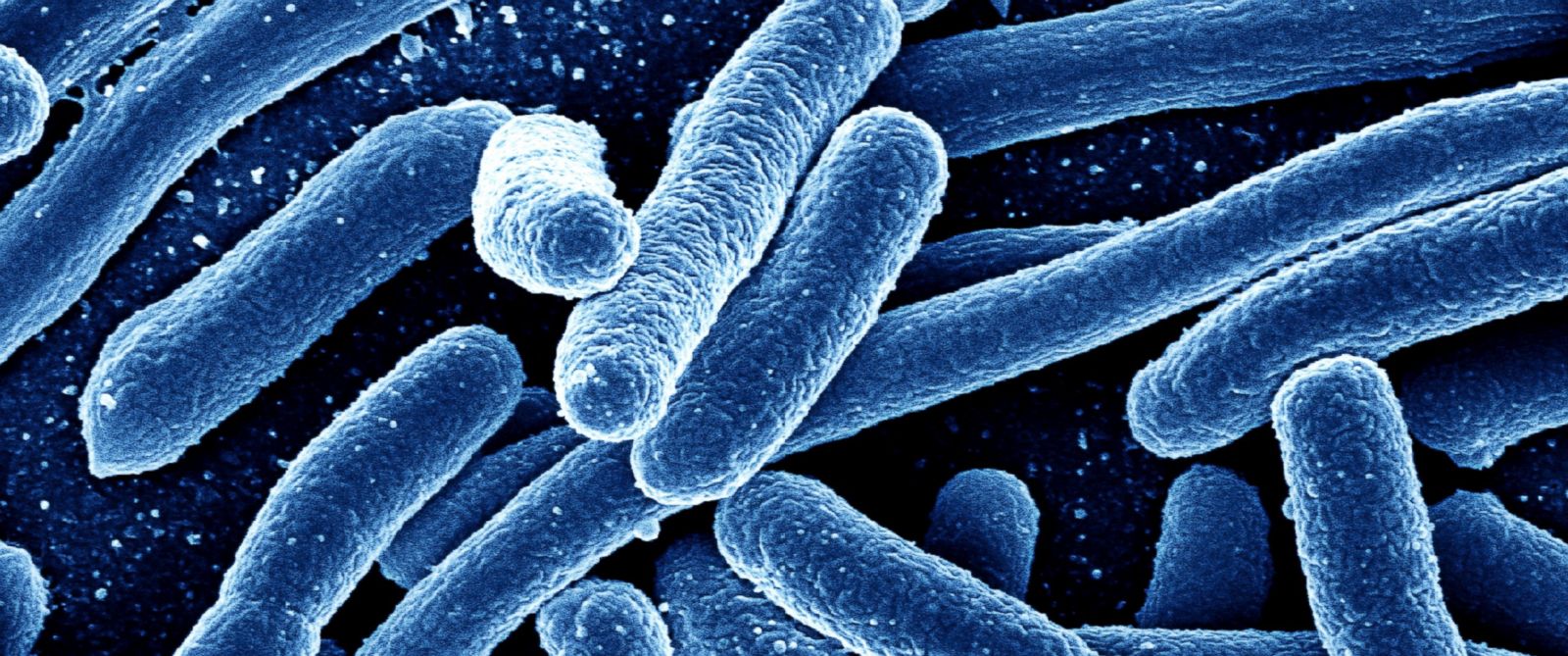
A study published in the online journal mBio revealed that the malaria-causing parasite Plasmodium vivax infects its hosts much, much deeper than previously thought. Researchers found evidence that the parasite penetrates as deep as the bone marrow where it often stays undetected and unimpeded from starting and spreading disease.
The World Health Organization (WHO) reports that of the 216 million cases of malaria around the world in 2016, about 445,000 ended in death. The disease is caused by plasmodia, microscopic parasites that victimize blood cells.
The parasites are transmitted by the bite of Anopheles mosquitoes, which pick up the microorganism from infected carriers they have previously bitten. Like other blood-transmitted diseases, malaria can be passed on through blood transfusions, organ transplants, and sharing needles and syringes. An infant can also inherit the disease from an infected mother in a case called congenital malaria.
There are four known parasites responsible for causing the condition. Among them, Plasmodium falciparum is the deadliest, causing around 90 percent of deaths.
P. vivax is known as the “benign” malaria not because its infection results in fewer deaths, but because it causes little to no symptoms. Blood tests on its hosts also detect low parasite numbers. Scientists now know why. (Related: Drug-resistant Malaria? Medication has failed for the first time.)
When malaria-causing parasites enter the human body, they proceed to the liver where they mature. After several days, they enter the bloodstream and infect red blood cells, inside which they multiply. They kill the cell by bursting it open and then look for other cells to attack. It is this savage cycle that causes the symptoms attributed to malaria.
The search for P. vivax
In the case of P. vivax, the researchers believe that the parasites form a reservoir inside the bone marrow where even current blood tests cannot detect them. This explains why very few parasites are usually found in the blood.
“We suspected there was a parasite reservoir somewhere in the body, and nobody had found it yet,” said senior author Matthias Marti, professor at the Harvard T.H. Chan School of Public Health and the University of Glasgow‘s Institute of Infection, Immunity & Inflammation.
Suspicions of the reservoir being in the bone marrow arose after observations that P. vivax often targeted young blood cells. The bone marrow is responsible for the production of blood cells.
To confirm their hypothesis, the researchers analyzed P. vivax’s transcriptome to identify the blood-borne proteins that act as markers corresponding to every stage of the microbe’s life cycle. They then searched for these markers in blood samples from infected patients.
They discovered that the blood samples did not represent a large portion of the parasites’ life stages. This meant that these stages occurred and accumulated in another area of the body.
The team then studied infected tissues from 13 non-human primate sources (malaria can also infect apes). These tissues included subcutaneous fat, brain, intestine, liver, lung, and bone marrow. The first three yielded few to no parasites, but an examination of the last three revealed antibody reactions to all stages of P. vivax’s life cycle.
Examination of the liver and bone marrow also located parasites outside of blood vessels. The scientists estimated that these two organs alone represented 30 percent of the animals’ parasite burden or the total number of parasites. Further studies are being conducted on how malaria develops inside the bone marrow.
The study’s findings are crucial to the development of blood tests that are more capable of finding hidden agents of malaria and other diseases.
“The study opens up a new area of investigation,” Marti said.
Learn more about malaria and other parasite-related diseases at Outbreak.news.
Sources include:
Tagged Under: anopheles, bone marrow, Diseases, infectious diseases, Malaria, mosquito, outbreak, P falciparum, p vivax, parasites, plasmodium, research, science